Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Multiple Primary Spinal Extradural Hydatid Cysts: A Clinical Case Report
*Corresponding author: Najeeb Ullah, Associate Professor, Institute of Basic Medical Sciences, Khyber Medical University, Peshawar, Pakistan.
Received: June 24, 2024; Published: June 28, 2024
DOI: 10.34297/AJBSR.2024.23.003043
Introduction
Spinal hydatid disease is an uncommon manifestation of hydatid disease. Growth of the parasite is generally slow in hydatid cyst arising from vertebral bone and is characterized by aggressive bone infiltration. We report a histopathologically confirmed primary recurrent hydatid disease of spinal cord in a 26-year-old lady presenting with lower limb weakness with an intention to have better understanding of this rare but clinically challenging disease. MR features were suggestive of caries spine with multicystic prevertebral, paravertebral, psoas muscle and intraspinal fluid collection accompanied by involvement and collapse of LV3 body. In conclusion, within endemic regions which includes south Asia, patients belonging to under privileged strata of the society with limited financial resources, spinal hydatid cyst is an important differential diagnosis in spinal cord compression syndrome.
Keywords: Hydatid cyst, Psoas abscess, Spinal cord compression
Introduction
Hydatid disease or cystic echinococcosis is caused by larval stage of tapeworm Echinococcus granulosis [1]. Two distinct mammalian hosts are required to complete the Life cycle of echinococcus, dogs as definitive hosts and humans as intermediate hosts [2]. Disease occurs in human through oro- fecal route. Hydatid disease most frequently involves liver and lung [3]. Secondary involvement of any anatomic location e.g. lung, spleen, brain, bone may be seen due to hematogenous spread except teeth, nail and hair [4,5]. Involvement of musculoskeletal is secondary and uncommon in hydatid disease Bone involvement is 0.5-2% of reported cases and 50% of these cases occur in spine [6].
Pelvis, sacrum, metaphyses of long bones, skull, spine and ribs are involved in hydatid disease in decreasing order of incidence. The incidence of spinal involvement is less than 1% of all cases of hydatid cysts [7,8]. Thoracic, Lumbar, and cervical regions are affected respectively [6]. It usually begins primarily as a single cyst which later contain daughter cysts. Sometimes these cysts may rupture into adjacent muscles forming secondary cysts. These cysts may also be forced by muscle movements some distance along vertebral column or in connective tissue planes [9].
Grossly the cyst is composed of semitransparent whitish yellow inner germinal layer and ivory white outer acellular or laminated membrane. External most fibrous layer is formed by host reaction to cyst. Hydatid cyst of bone grows continuously in cancellous bone in outward direction causing destruction and resorption leading to exogenous cysts. Therefore, pericyst or fibrous layer does not form in the bone hydatid cyst [10]. Cells of germinal layer proliferate forming protoscolex, having retractile hook lets. These can be seen in histological sections. The proto scolices grow into brood capsules with in a vesicle of germinal membrane. Rupture of brood capsules may drop the larvae into fluid. The sediment of fluid (hydatid sand) comprises of protoscolices, brood capsules and hooklets. Seepage of this fluid will cause inflammatory reaction or granulomatous inflammation. Brood capsules which remain attached to germinal layer grow to form daughter cysts. Degeneration and calcification occurs in others. Protoscolices are infective for definitive host. On histology laminated layer stains amphiphilic with H and E stain and outer layer is adventitial layer [11].
Hydatid disease in spine is a rare condition having poor prognosis and literature generally shows regional publications. Neurological complications relate to the severity of disease-causing compression of spinal cord [12]. We report a histopathologically confirmed primary hydatid disease of spinal cord in a 26 year old lady presenting with lower limb weakness and brief review of the relevant literature.
Patient came through OPD with history of low backache, pain in both lower limbs for 04 years. Pain was exaggerated with walking and was associated with paraesthesia. O/E: Patient was walking with support and painful lumbar movements. MR features were suggestive of caries spine with multicystic prevertebral, paravertebral, psoas muscle and intraspinal fluid collection accompanied by involvement and collapse of LV3 body. U/S Abdomen/Pelvis: shows bilateral psoas abscesses. Per operatively L3, L4 PID with multiple hydatid cysts seen. Large hydatid cyst was communicating to spine and left psoas muscle. L3, L4 decompressive laminectomy for multiple hydatid cysts done. Transpedicular screw fixation using titneum plates was done.
Histopathological evaluation shows three layers of hydatid cyst. The inner most germinal layer is thin. The embryonic tape worm, scolices, develops from an out pouching of the germinal layer and form hydatid sand, settling into the dependent parts of cyst (Figure 1). She was given albendazole 2 tablets twice daily for 2 months.
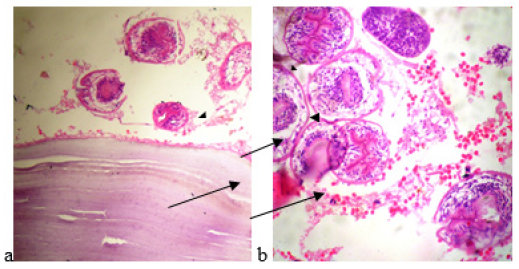
Figure 1: The cyst wall is composed of a cellular laminated membrane (long arrow) and an inner nucleated germinal layer (arrow). Protoscolices and brood capsule (arrowhead) are present.
After five years she was admitted again through OPD with the history of low back pain for the last 02 months. Pain associated to left lower limb for the same period of time. O/E Her GCS: 15/15.Planters: Bilateral down going. Power: moving all limbs. Sensory/ Motor system intact. Reflexes: normal. Abdomen: soft non tender. Chest: Clear Ct scan chest with contrast showed collapse of LV3 with reduced adjacent disc spaces, mixed lytic and sclerotic lesions in the LV2 and LV4 with some end plate irregularity and collections within the bilateral psoas muscles along with loculated ascites. Important differential diagnosis would include spinal tuberculosis and hydatid disease.
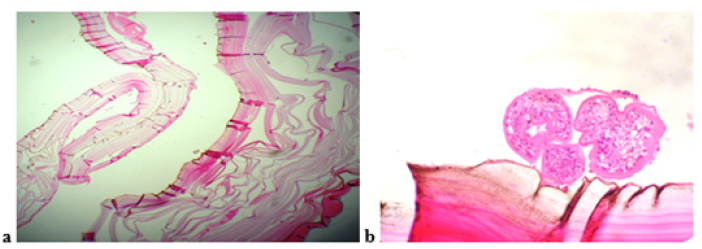
Figure 2: A cellular laminated membrane of the cyst wall (a). Protoscolices and brood capsule are also present (b).
Previous CT abdomen and pelvis examination was also reviewed for comparison. There is redemonstration completely collapsed fragmented body of L3 vertebra with severe spinal canal stenosis. Redemonstration associated loculated collection in bilateral psoas muscles and prevertebral location. She underwent anterior decompression of L3 vertebral body and multiple hydatid cysts were removed. Hypertonic saline solution was used during surgery. Histological examination confirmed the hydatid cysts (Figure 2).
She was given Tab vermox 100mg 3 times a day for 3 months. She was also advised not to share room with cattle and goats. Follow up is done yearly since then and she is disease free now for the last 8 years.
Discussion
Hydatid cyst has been reported around the world at unusual sites as spleen, kidney, heart, bones, muscles and cranium [13]. Involvement of spine is unusal and was first reported by Churrier in 1807 [14]. Disease usually spread by direct extension from abdominal, pulmonary or pelvic infestation. Primary vertebral hydatid disease occurs due to direct portovertebral venous shunts and tendency of the parasite to grow easily in cancellous bone [6]. In the literature one third patients had previous surgical history for their cysts [8]. Our patient had no history of cyst resection. Growth of hydatid in cancellous bone occurs in outward direction causing destruction and resorption by pressure necrosis and resorption leading to exogenous cyst formation. Thoracic spine is most commonly involved (50%), followed by lumbar (20%), sacral (20%) and cervical spine (10%) [6]. In our case lumbar spine is involved. Previously the reported incidence in lumbar vertebrae is a little higher [8,15].
Mediterranean countries, the Middle East, South America, New Zealand, Australia, and Southeast Asia and many parts of china are endemic for hydatid disease where sheep, dogs and man live in close contact [16]. Pakistan is also an endemic area to the disease because of close association of people with sheep and dogs [17]. Therefore, spinal hydatosis although rare; in endemic areas physcians should be vigilant enough in cases of patients with mild symptoms to include it in differential of causes of low back problems. The disease can be easily confused with tuberculous spondylitis and tuberculosis is endemic too. Misdiagnosis could lead to serious consequences.
Symptoms of spinal hydatid cyst are of slowly growing mass situated in the dorsal region causing radicular symptoms or symptoms of cord compression leading to various degrees of limb weakness like paresthesia, paraperasis, paraplegia and sometimes sphincter dysfunction [18]. Our patient presents with weakness of limbs which improved significantly following surgery.
In 1981 Braithwaite and Lees classified spinal hydatid disease in five groups [19] as follows:
a) Primary intramedullary hydatid cyst
b) Intradural extramedullary hydatid cyst
c) Extradural intraspinal hydatid cyst
d) Hydatid disease of the vertebra
e) Paravertebral hydatid disease
Our case was an example of Type 3 variety. The most beneficial method for prompt diagnosis of spinal hydatid disease is MRI [20]. Precise level of location and its extension into paraspinal tissue is characterized on MRI. MRI is therefore superior in the diagnosis of spinal hydatid disease than CT [20]. Tuberculous spondylitis and chronic osteomyelitis are easily confused with spinal hydatid disease. Some imaging characteristics are described as pathogenic of Spinal hydatid disease such as absence of sclerosis and osteoporosis, lack of damage to disk space and vertebral bodies and paraspinal extensions. In our case MRI show soft tissue masses in paraspinal muscles. They are spherical, fluid filled cysts. Vertebral lesions appear as intraspinal extensions causing bone sequestration and paravertebral cysts. Spinal hydatid cyst unlike brain cyst demonstrates no rim enhancement after injection of contrast material. Presence on T1 and T2 weighted images of hypointense cyst wall is characteristic of hydatid disease [6].
Ultrasonography of abdomen done in our case did not show any involvement of abdominal organ in the disease process. Diagnosis of hydatid cyst should be considered for cystic lesions causing cord compression, confirmation is done by surgical exploration. The operative choice for spinal hydatid cyst is laminectomy although anterior vertebrectomy also gives good results in causing decompression [8]. Surgical approach is affected mainly by degree of spinal canal involvement [21]. Recurrence remains a major problem in hydatid disease of spine (30-100%) and it also correlates with cyst location [18,21]. Use of hypertonic saline solution during surgery has been recommended to prevent recurrences. long term follow up with radiographs and serological tests should be done periodically to ensure any recurrence.
Conclusion
Spinal hydatid disease, although rare in developed countries, must be considered in the differential diagnosis of spinal cord compression syndrome especially in endemic areas. Despite aggressive treatment, overall outcome is poor leading to a prognosis measured by years.
Acknowledgement
We acknowledge the support of the IBMS-KMU, ORIC-KMU as well as the support of Northwest General Hospital and Research Centre by providing access to the labs for performing our experiments.
Conflict of Interest
The authors declare no conflict of interest.
References
- Parija SC (2004) A Textbook of Medical Parasitology 2nd All India Publishers and Distributors: 220-229.
- Paredes R, Godoy P, Rodriquez B, Garcia MP, Cabezon C, et al. (2011) Bovine (Bostaurus)humoral immune response against Echinococcus granulosus and hydatid cyst infertility. J Cell Biochem 112(1): 189-199.
- Mondal SK, Sengupta SG (2009) Hydatid cyst of radial bone. JNMA J Nepal Med Assoc 48(176): 321-323.
- Polat P, Kantarci M, Alper F, Suma S, Koruyucu MB, et al. (2003) Hydatid disease from head to toe. Radiographics 23(2): 475-494.
- Ismail MA, Al Dabagh MA, Al Janabi TA, M I Al Moslih, M S Al Ani, et al. (1980) The use of computerized axial tomography in the diagnosis of hydatid Hydatid cyst. Clin Radiol 31(3): 287-290.
- Awasthy N, Chand K (2005) Primary hydatid disease of spine: An unusual case. Br J Neurosurg 19(5): 425-427.
- Fares Y, Khazim R, El Zaatari MM, Haddad GF, Bannes PR (2003) Spinal hydatid disease and its neurological complications. Scand J Infect Dis 35(6-7): 394-396.
- Pamir MN, Akalan N, Ozgen T, Erbengi A (1984) Spinal hydatid cyst. Surg Neurol 21(1): 53-57.
- Fiennes AG, Thomas DG (1982) Combined medical and surgical treatment of spinal hydatid disease:a case report. J Neurol Neurosurg Psychiatry 45(10): 927-931.
- Begggs I (1985) The radiology of hydatid disease. Am J Roentgenol 145(3): 639-648.
- Gutierrez Y (2000) The Cestode.In :Diagnositic pathologyof parasitic infections with Clinical Correlation.2nd ed: 676-677.
- Zaalouni I, Quertatani M, Meherzi MH, Ben Hamida MK, Rbai H, et al. (2010) Costovertebral echinococcosis a case report and review of the literature Rev Med Interne 31(1): 69-71.
- Cangiotti L, Muiesan P, Begni A, de Cesare V, Pouche A, et al. (1994) Unusual localization of hydatid disease: a 18 year experience.G Chir 15(3): 83-86.
- Rayport M, Wisoff HS, Ziman H (1964) Vertebral echinocossosis. J Neurosurg 21: 647-59.
- Bavbek M, Inci S, Tahta K, Bertan V (1992) Primary multiple spinal extradural hydatid cysts. Case report and review of the literature. Paraplegia 30(7): 517-519.
- Eroglu A, Atabekoglu H (1999) Primary hydatid cyst of neck. Eur Arch Otorhinolaryngol 256: 202-204.
- Hussain A, Maqbool A, Hussain S, Athar M, Shakoor A, et al. (1992) Studies on prevalence and organ specificity of hydatosis in ruminants slaughtered at Karachi and Faisalabad abattoir. Pakistan. Indian J Dairy Sci 45: 454-456.
- Berk C, Ciftci E, Erdogan A (1998) MRI in primary intrspinal extradural hydatid disease: Case report. Neuroradiology 40: 390-392.
- Brathwaite PA, Lees RF (1981) Vertebral hydatid disease. Radiological assessment. Radiology 140(3): 763-766.
- Islekel S, Ersahin Y, Zileil M, N Oktar, K Oner, et al. (1998) Spinal hydatid disease. Spinal cord 36(3): 166-170.
- Rahimi Jaberei A, Farrokhi HR, Sharifian Dorche M, Nikseresht AR (2012) Hydatid disease of the spine: a case report. Shiraz E Medical Journal: 13(2).



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.